Not all plaque in your arteries is equally dangerous. To lower your heart attack risk, it helps to know what's actually inside those plaques – and which ones you should target first.
Coronary plaques fall into three categories:
 Calcified plaque: made mostly of hardened calcium. These are the most stable and the least likely to rupture and cause a heart attack. They only cause about 8-12% of thrombotic heart attacks.
Calcified plaque: made mostly of hardened calcium. These are the most stable and the least likely to rupture and cause a heart attack. They only cause about 8-12% of thrombotic heart attacks. Non-calcified plaque (often called soft plaque): contain fibrous tissue and some fat. These can pose moderate risk, but they're not as dangerous as low-density plaques.
Non-calcified plaque (often called soft plaque): contain fibrous tissue and some fat. These can pose moderate risk, but they're not as dangerous as low-density plaques. Low-density non-calcified plaque (often called high-risk soft plaque): made up mostly of fat and loose connective tissue. These are the most dangerous because they're far more likely to rupture, leading to a sudden clot that can block an artery completely.
Low-density non-calcified plaque (often called high-risk soft plaque): made up mostly of fat and loose connective tissue. These are the most dangerous because they're far more likely to rupture, leading to a sudden clot that can block an artery completely.
Soft plaques – especially low-density non-calcified plaques – are the main cause of unexpected heart attacks in people who otherwise feel fine.
In this article, you'll learn how to identify and aggressively treat soft plaque, before it can break open and do damage.
How to Stage Atherosclerosis with CCTA
A recent expert consensus paper published in The American Journal of Medicine introduced the Atherosclerosis Treatment Algorithms. These treatment algorithms use an atherosclerosis staging system for classifying coronary artery disease by disease burden, as seen below.
| Stage Description | TPV (mm³) | PAV (%) | Medical Therapy | Possible Examples |
|---|---|---|---|---|
| Stage 0: No Plaque | 0 | 0 | May not be necessary | Baseline guided directed medical therapy (GDMT) |
| Stage 1: Mild Plaque | >0 to 250 | >0 to 5% | Guideline directed medical therapy (GDMT) | Statins. Ezetimibe. |
| Stage 2: Moderate Plaque | >250 to 750 | >5 to 15% | Moderately intensive | High Intensity Statins. Ezetimibe. Rivaroxaban. Aspirin. Inclisiran. Bempedoic Acid. Others. |
| Stage 3: Severe Plaque | >750 | >15% | Most intensive | High Intensity Statins. Ezetimibe. Rivaroxaban. Aspirin. PCSK-9 Inhibitor. Colchicine. Icospaent Ethyl. Inclisiran. Bempedoic Acid. Others. |
These new guidelines give doctors personalized recommendations for medical therapy based on two things:
 Your CCTA scan results (which measure actual plaque volume)
Your CCTA scan results (which measure actual plaque volume) Your traditional cardiovascular risk factors (like cholesterol, blood pressure, and smoking)
Your traditional cardiovascular risk factors (like cholesterol, blood pressure, and smoking)
To our knowledge, it's the first pathway that directly ties plaque severity and progression to real-world recommendations for which medications to start – and when to adjust them.
This means patients finally have a roadmap that connects what's actually inside their arteries with what they should do about it.
Here's how it works:
Total plaque volume refers to the overall amount of plaque inside your arteries, usually measured in cubic millimeters (mm³). It's a big-picture marker of how far atherosclerosis has progressed.
Percent atheroma volume (PAV) shows how much of a vessel is filled with plaque. It's calculated as: (total plaque volume ÷ total vessel volume) × 100. This number is important because higher PAV is strongly linked to a higher risk of cardiovascular events.
These measurements can all come from a Coronary CT Angiography (CCTA) with an AI-powered analysis like HeartFlow or Cleerly.
So what raises your risk for building up more plaque in the first place? Key risk factors include:
- High cholesterol and triglycerides
- High blood pressure
- Smoking
- Type 1 or Type 2 diabetes
- Obesity
- Physical inactivity
- A diet high in saturated fats
- Family history of atherosclerosis
- Older age, especially 55 and up
The takeaway: CCTA plaque staging enables much more targeted, aggressive medical therapy to actually reduce your heart attack risk.
Atherosclerosis Treatment Algorithms
So – you (or your patient) have staged your plaque burden. Now what? What exactly do you do next to stop progression or even reverse soft plaque?
Treatments that target plaque regression fall into two broad buckets:
 Dietary and lifestyle changes
Dietary and lifestyle changes Pharmacological therapy
Pharmacological therapy
While lifestyle is the essential foundation, medications have had by far the biggest impact on shrinking or stabilizing plaque – so that's where we'll focus here.
Treatments targeting plaque regression can broadly be divided into 2 main categories:
1) Dietary and lifestyle.
2) Pharmacological (Central Illustration). Pharmacological treatments have had by far the most success and form the majority of the discussion in this section.
Stage 0
Guideline-Directed Medical Therapy (GDMT)
If you're truly low risk, the goal is to stay that way:
- Keep blood pressure under control
- Maintain healthy cholesterol levels
- Manage blood sugar (especially if you have diabetes)
- Stick with proven lifestyle habits: heart-healthy diet, regular exercise, no smoking.
If your overall risk is genuinely low, you and your doctor may even decide to reduce or stop certain meds if the risk-benefit balance supports it.
Stage 1
Statins (Rosuvastatin 10–20 mg daily or Atorvastatin 20–40 mg daily)
What they do: Lower LDL cholesterol by reducing production in the liver and boosting LDL clearance.
Why it matters: Lower LDL means less plaque buildup. Statins also reduce inflammation, stabilize soft plaque, and help transform it into more calcified, stable plaque.
Ezetimibe (10mg daily)
What it does: Blocks cholesterol absorption in the gut.
Why it matters: Provides additional LDL lowering when statins alone don't get you to target or when statins are not tolerated.
Stage 2
All of Stage 1 plus:
High-Intensity Statin (Rosuvastatin 40 mg QD / Atorvastatin 80 mg QD)
What it does: Even greater LDL lowering (≥50% reduction); more potent effect on plaque stabilization and regression.
Aspirin (81–100 mg QD)
What it does: Antiplatelet agent – helps prevent clots from forming on top of a ruptured plaque.
Why it matters: Rupture and clotting is what turns plaque into a sudden heart attack or stroke.
Rivaroxaban (2.5 mg BID)
What it does: Low-dose anticoagulant that reduces the risk of clot formation in high-risk patients with chronic CAD/PAD.
Why it matters: Works synergistically with aspirin to lower major cardiovascular events.
If diabetic, GLP-1 receptor agonist
What it does: Lowers blood sugar, reduces weight, and has direct vascular protective effects.
Why it matters: Large trials show GLP-1 RAs reduce cardiovascular events in people with diabetes.
Stage 3
All of Stage 2 plus:
PCSK9 inhibitors (e.g., evolocumab, alirocumab)
What they do: Increase clearance of LDL particles by enhancing LDL receptor recycling.
Why it matters: Up to 60% extra LDL reduction on top of statins; proven to reduce major cardiovascular events in very high-risk patients.
Icosapent ethyl (e.g. Vascepta) – optional
What it does: Highly purified EPA omega-3 that lowers triglycerides and has anti-inflammatory effects; reduces CV events independent of LDL.
Why it matters: In adults with triglycerides ≥150 mg/dL and established CVD or diabetes and ≥2 CVD risk factors, Vascepta lowered the chance of a life-threatening cardiovascular event (such as a heart attack or stroke) by 25% when added to a statin.
Bempedoic acid – optional
What it does: Inhibits cholesterol synthesis upstream of statins but works only in the liver (less muscle side effects).
Why it matters: Good option for patients who can't tolerate high-dose statins.
Colchicine 0.6 mg QD – optional
What it does: Suppresses vascular inflammation by blocking the NLRP3 inflammasome pathway.
Why it matters: Low-dose colchicine has been shown to safely lower major adverse cardiovascular events by 31% among those with stable atherosclerosis and by 23% after recent myocardial infarction.
Cardiac rehab / supervised exercise
What it does: Improves endothelial function, lowers inflammation, helps weight and blood pressure, and reduces mortality after heart events.
Applying the Staging and Treatment Guidelines: Patient A
Let's look at how this works in the real world.
Patient A is a 62-year-old male with:
- Type 2 diabetes
- BMI of 27 (overweight)
- LDL of 60 (normal)
- A1C of 6.4% (slightly elevated; normal is below 5.7%)
- Normal blood pressure
- 20 pack-year smoking history, but quit 10 years ago
- Family history of high cholesterol, high blood pressure, and type 2 diabetes
Three years ago, Patient A discovered he had a Coronary Artery Calcium (CAC) score of 1,000, which made him incredibly worried. This CAC score prompted him to get a cardiac catheterization that showed 20–29% stenosis in his LAD artery. His cardiologist told him: "You're good to go – nothing to worry about!"
Where does he stand now?
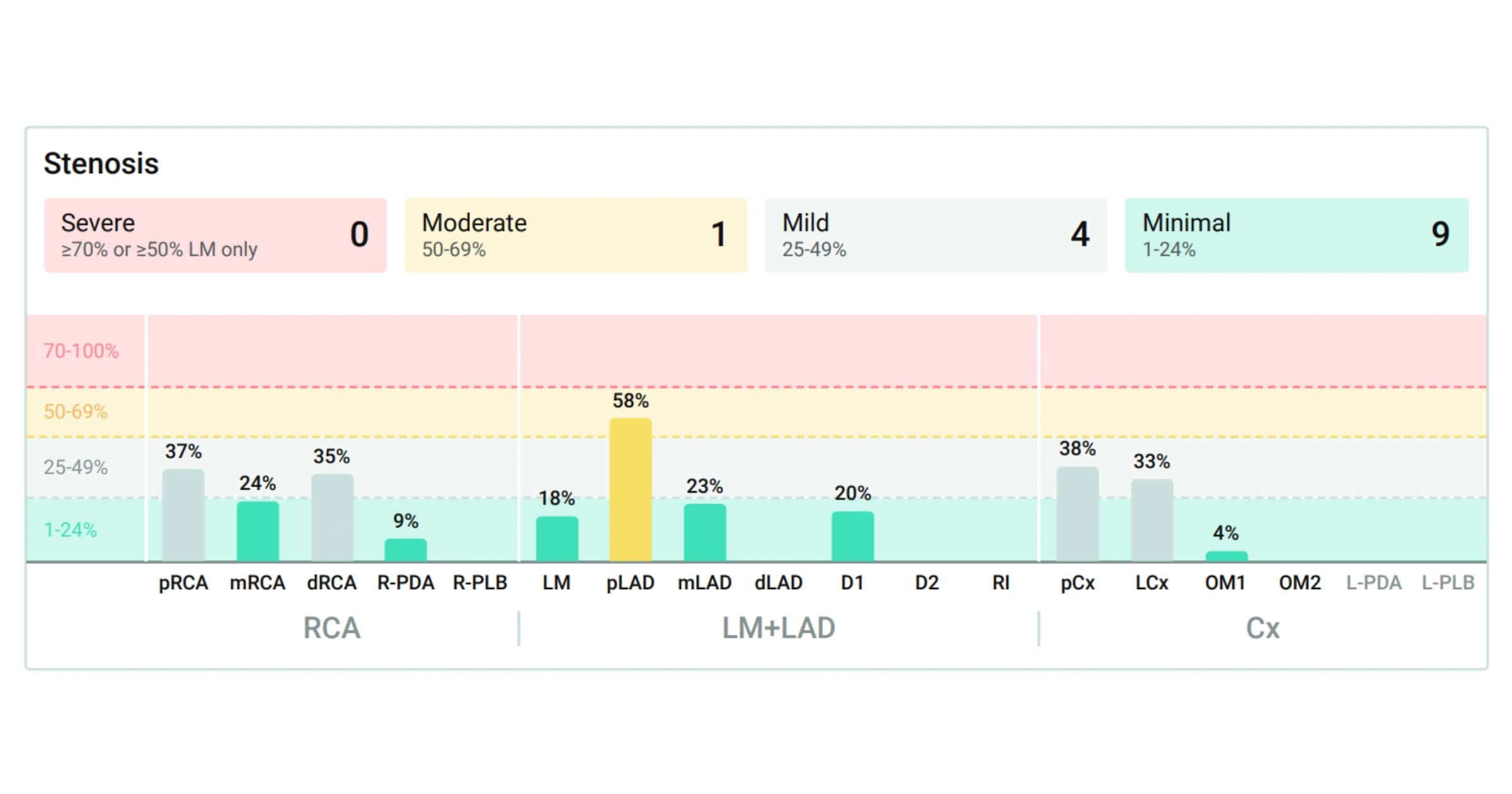
Patient A got a CCTA with AI plaque analysis that showed the following results:
| Territory | Low-Density Soft Plaque Volume (mm³) | Soft Plaque Volume (mm³) | Hard Plaque Volume (mm³) | Total Plaque volume (mm³) | Percent Atheroma Volume |
|---|---|---|---|---|---|
| RCA | .3 | 189.4 | 210.3 | 400 | 22.1% |
| LM+LAD | .3 | 144.9 | 231 | 376.2 | 30.7% |
| Cx | .1 | 46.1 | 18.6 | 64.8 | 10.5% |
| Total | .7 | 380.4 | 459.9 | 841 | 23% |
Analyzing these results, we can see that:
- Total plaque burden: 841 mm³ = Stage 3 atherosclerosis (above the 750 mm³ threshold)
- Percent atheroma volume (PAV): 23% = also Stage 3 (above the 15% threshold)
- Low-density non-calcified plaque: 0.7 mm³
- Non-calcified plaque: 380 mm³
- Calcified plaque: 480 mm³
Only one vessel – the LAD – shows significant stenosis: 58%.
What did the cath miss?
The invasive cath didn't show any soft plaque behind the artery wall. It didn't detect his true risk. Likewise, his CAC score told him he had a lot of calcified plaque – but not that he also has a big burden of soft plaque, which is much more dangerous.
Key point:
- Calcified plaque is less of a concern – it's stable, unlikely to rupture, and only causes ~8–12% of thrombotic heart attacks.
- The real threat is the soft, lipid-rich plaque – responsible for most heart attacks – and the moderate stenosis that could worsen.
What's the goal for Patient A?
 Target: The 380 mm³ of soft plaque and 0.7 mm³ of low-density, high-risk soft plaque – especially in the LAD lesion with 58% stenosis.
Target: The 380 mm³ of soft plaque and 0.7 mm³ of low-density, high-risk soft plaque – especially in the LAD lesion with 58% stenosis. Strategy: Use aggressive medical therapy to: Convert or remove soft plaque (shrink it, stabilize it, and help it calcify), Reduce stenosis to keep blood flow strong, Minimize risk of plaque rupture and clot formation
Strategy: Use aggressive medical therapy to: Convert or remove soft plaque (shrink it, stabilize it, and help it calcify), Reduce stenosis to keep blood flow strong, Minimize risk of plaque rupture and clot formation
This picture from his CCTA with Cleerly AI shows the LAD artery with the 58% stenosis:
Blue = calcified plaque
Yellow = soft plaque

Until now, it was impossible to analyze each individual plaque lesion in detail. An invasive cath can't show the full picture – it only reveals how narrow an artery is (stenosis), not what's hidden behind the wall (plaque).
And a calcium score alone would only pick up the hardened plaque, missing the larger burden of soft, high-risk plaque entirely.
So a lesion like this might look harmless with standard tests – but in reality, it needs targeted treatment.
Treatment
Before his CCTA, Patient A was already on a few medications:
- Glucophage 1000 mg BID – to help control blood sugar
- Metoprolol 50 mg BID – to keep blood pressure and heart rate in check
- Crestor (rosuvastatin) 20 mg daily – to reduce LDL cholesterol
After seeing his CCTA results, the plan was to keep those baseline meds the same – but add targeted new therapies to aggressively tackle his soft plaque:
 Repatha (PCSK9 inhibitor) 140 mg every 2 weeks
Repatha (PCSK9 inhibitor) 140 mg every 2 weeks
Goal: drop LDL well below 60 mg/dL, ideally closer to <20 mg/dL for maximum plaque regression. Aspirin 81 mg daily
Aspirin 81 mg daily
Helps prevent blood clots from forming on any unstable plaque. GLP-1 receptor agonist (Ozempic 0.25–0.5 mg)
GLP-1 receptor agonist (Ozempic 0.25–0.5 mg)
Goal: lower BMI, bring A1C down further, and support soft plaque remodeling.
The plan is to repeat his CCTA in 12 months to see exactly how much plaque volume and stenosis have changed. In the meantime, he was encouraged to continue improving his diet and maintain a more active lifestyle – the foundation that makes medications work even better.
His Crestor dose wasn't increased to 40 mg just yet – the idea is to see how much progress the new meds make first. (Though in some cases, pushing statin intensity further would be reasonable, too.)
Conclusion
As you can see, applying these staging and treatment guidelines helps people move from vague risk estimates to clear, actionable steps to reduce their chance of a heart attack. By actually characterizing plaque, we can make smarter decisions about when to pursue aggressive medical therapy – instead of guessing.
This shows just how powerful CCTA can be for non-invasively screening and managing CAD. If you missed it, we covered exactly how CCTA stacks up against every other CAD screening test in our guide: Ranking Every Test for Heart Attack Risk.
Patient A is the perfect example of how this works in real life:
- He was cath negative and had a high calcium score, yet three different cardiologists told him he was fine.
- Meanwhile, his soft plaque was growing, and he developed a 58% stenotic lesion that no one saw – until his CCTA.
- Now, with clear data, he's on aggressive medical therapy to shrink that soft plaque and stabilize his arteries – giving him a real shot at preventing a future heart attack.
 In 12 months, we'll repeat his CCTA and share the results – so you can see exactly what changed.
In 12 months, we'll repeat his CCTA and share the results – so you can see exactly what changed.
I hope this guide inspires you to take charge of your own cardiovascular health.
This article is for informational purposes only and is not intended as medical advice. Always consult your doctor before making any changes to your treatment plan.
Sources
[1] Nurmohamed, N. S., Bom, M. J., Jukema, R. A., de Groot, R. J., Driessen, R. S., van Diemen, P. A., de Winter, R. W., Gaillard, E. L., Sprengers, R. W., Stroes, E. S. G., Min, J. K., Earls, J. P., Cardoso, R., Blankstein, R., Danad, I., Choi, A. D., & Knaapen, P. (2024). AI-Guided Quantitative Plaque Staging Predicts Long-Term Cardiovascular Outcomes in Patients at Risk for Atherosclerotic CVD. JACC. Cardiovascular imaging, 17(3), 269–280. link
[2] Centers for Disease Control and Prevention. Heart Disease Facts. Last reviewed February 7, 2022.
[3] Centers for Disease Control and Prevention. Interactive Atlas of Heart Disease and Stroke. 2.
[4] Journal of Cardiovascular Computed Tomography. Coronary CTA Plaque Volume Severity Stages According to Invasive Coronary Angiography and FFR. Published March 28, 2022
[5] Nelson, K., Fuster, V., & Ridker, P. M. (2023). Low-Dose Colchicine for Secondary Prevention of Coronary Artery Disease: JACC Review Topic of the Week. Journal of the American College of Cardiology, 82(7), 648–660. link